Have to be Painful
Downloadable Info Sheet
The Employer’s Guide to COBRA
Benefits Outsourcing 101: COBRA Administration
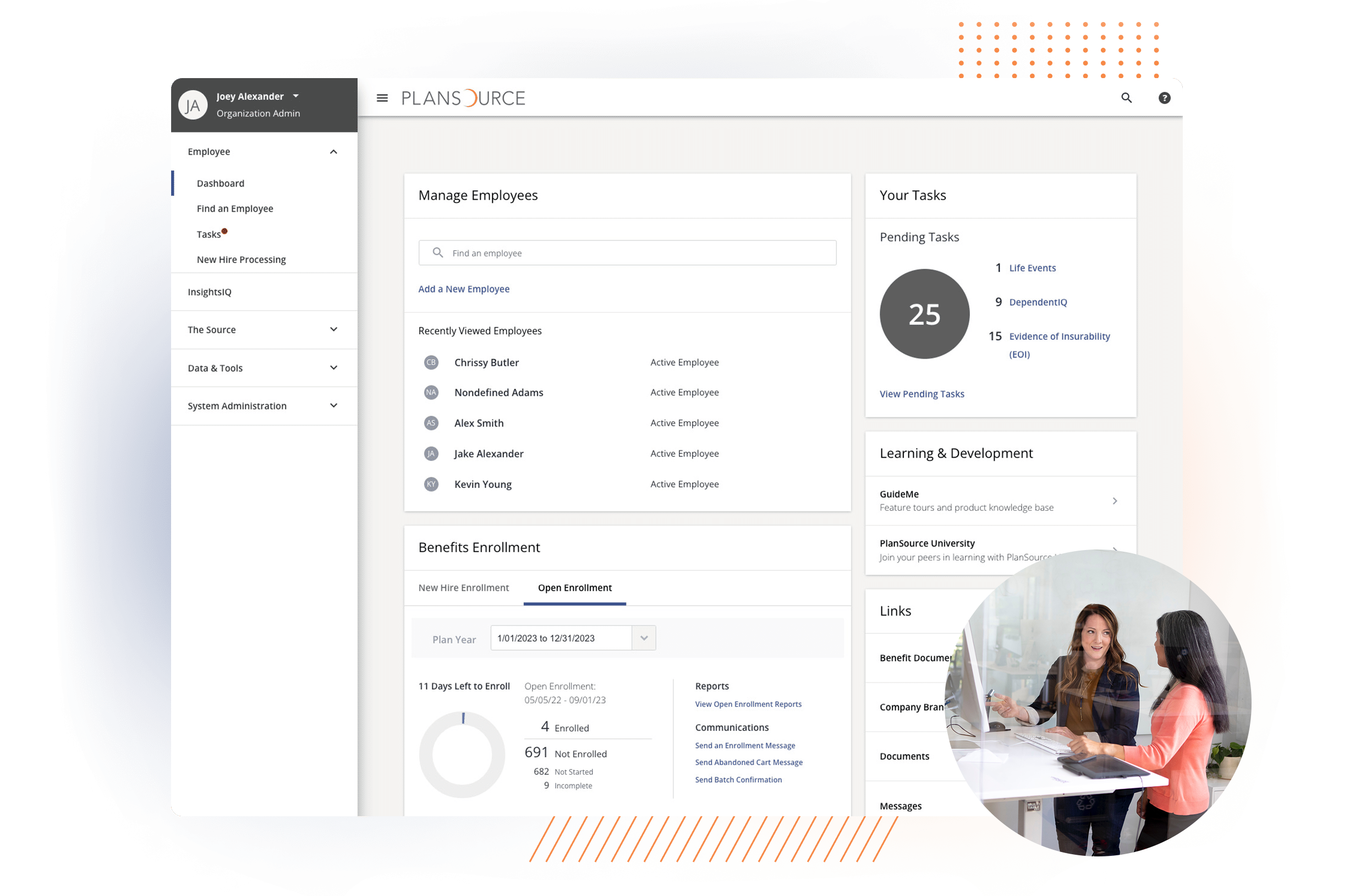
System Configuration and Maintenance
New Hire, Life Event and EOI Processing
Data Exchange Operations, Auditing and Reconciliation
COBRA Administration
Billing Reconciliation and Payment Services
Eligibility Management and Urgent Coverage Resolution
Branded Employee Contact Center

Chris Forbeck
