
That is why PlanSource has set out to revolutionize the benefits industry and create the customer experience of the future with simplified billing, an optimized consumer experience and modern, real-time API integrations with leading insurance carriers.

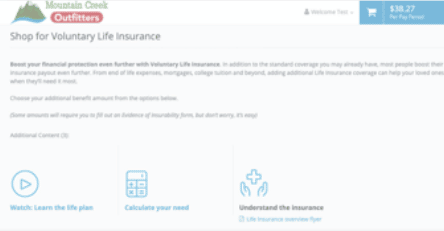
The Boost APIs are so easy to use. All the info pulled over from the carrier, including voluntary plans with age-banded rates and complex rules. It was automatically configured and 100% accurate! I love the new videos and page content for employees, too!

Available Now: Guardian
“Prior to having the EOI integration in place I was chasing down employees for 3 months trying to get the forms completed. This year all forms were completed right away during the shopping experience! It’s amazing!” – Broker
Available Now: Cigna, Guardian, MetLife, Prudential
SSO Available Now: The Hartford, Lincoln, Unum, Voya
Available Q2 2021: Guardian
Available for: Guardian, MetLife
Eliminates the need to reconcile carrier bills. Saves customers on average 40 hours a month
- Boost carriers no longer need to track and send bills to customers
- PlanSource collects premium from customers and pays the carriers directly
- Customers receive one consolidated bill for all Boost products










Open Enrollment Communications Kit
Engaging and Empowering Employees with Data and Insights
Join us for an enlightening webinar with Stacey Harris, Chief Research Officer at Sapient Insights Group, and Tamra Miller, Benefits Manager at Ingevity, as we delve into the transformative power of data and insights in the workplace. Don’t miss this opportunity to gain valuable insights and actionable strategies to support your HR team and empower your workforce!

